CORONARY VESSELS & RELEVANT INVESTIGATIONS Part - II
- Apr 13, 2025
- 15 min read
Updated: May 2, 2025
Initially nonspecific treatment was advised for relieving symptoms due to exertional angina. Physicians believed that a direct restoration of circulation and correction of the demand/supply need of the regional myocardial tissue will lead to a recovery. Surgical single artery aorto-coronary bypass was attempted first and the names of Rudolph Hoess and Sabiston stand out. With the passage of time Favalaro, Green, Lytle, etc. showed the invasive multi-vessel coronary bypass was feasible and improved the quality of life after recovery in patients with angina and deranged electrocardiogram. Vineberg directly implanted the left internal mammary artery (LIMA) into the left ventricular myocardium and Tector showed the possibility of increasing conduit length by anastomosing the two internal mammaries. Sequential grafting, alternative conduits and different grating methods and strategies were extensively debated and researched. Coronary bypass became one of the commonest surgical procedures of the millennium.
1977 saw Gruentzig introduce balloon angioplasty of stenotic coronary arteries and in 1986 Sigwart further bolstered the method by deploying stents in the balloon dilated stenotic areas. Percutaneous coronary intervention or (PCI) as it is commonly known, is catheter based and less invasive. PCI has competed with surgical revascularization and together these have become the major procedures for relieving coronary circulatory insufficiency. We are now debating the role of hybrid procedures where PCI can do the immediate circulatory restoration and surgical revascularization will ensure longevity.
Continued studies meanwhile led to better understanding of the pathophysiology of coronary insufficiency. Rahimtoola's theory of shocked and hibernating myocardium contributing to regional wall motion abnormality made surgeons understand that viable non-moving myocardial tissue could be successfully recruited for more effective ejection and prevention of heart failure. Sophisticated investigations were proposed to supplement the basic clinical findings, ECG, treadmill test, echocardiography done till recently for garnering mere information about the nature and extent of this condition. Management of patients with features of coronary insufficiency include revascularization either by PCI or surgery using conduits and maximum anti-angina and concomitant heart failure medicines. Again surgical revascularization can be on a still heart with pump support or on the beating heart. PCI is gaining because of its less invasive nature and fast recovery. Till recently those practicing revascularization were happy with a catheter based dynamic selective coronary angiogram, but of late clinicians are seeking further information with an aim at betterment of a patient and if lifestyle and dietary changes can slow a progressive process ensuring a better quality of life.
A summary of investigations in a logical sequence to be followed in coronary insufficiency follows:
1.ECG:- Automaticity is a unique quality of cells making up myocardial tissue and an Electrocardiogram (ECG) represents the surface potentials of the cardiac cells and the physicians are aware of the changes that occur with injury and infarction of heart tissue. ECG evolved over a long period and in 1909 Sir Thomas Lewis, after identifying a case of atrial
fibrillation (known as 'delirium cordis' at that time), recognised the implications of a change of the ECG pattern in infarction. He was instrumental in introducing ECG in clinical practice and with the introduction of augmented leads and 12 leads
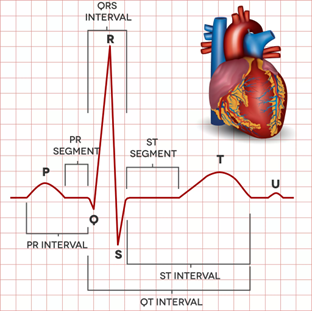


Nowadays ECG is one of the first tests that a cardiologist does for clinical evaluation of a patient. According to recent studies, with the application of artificial intelligence ECG has now become more informative.
Above are two examples of ST-segment elevation (STEMI) and non ST-elevation (NSTEMI) myocardial infarctions. Usually a downward depression of the ST segment of an ECG suggests insufficiency, while the upward coving of the same segment indicates tissue injury. Consistent deep Q-wave appearances and inversion or tenting of T-waves also suggest ischemia.
In some conditions, the first 12 lead ECG may not be suggestive and an ECG under some duress, i.e. under some protocolized exercise (commonly the Bruce protocol) of a metabolic equivalent tolerable according to the clinical profile of the patient in a treadmill, is followed. This is the treadmill test (TMT), and such a test may bring out ECG features of mismatch of circulatory demand and supply.
2. Echocardiography:-- Echocardiography, or cardiac ultrasound, is a non-invasive diagnostic process that uses specific sites and windows to capture the cardiac structures. evaluation. Reflective streams of ultrasound waves are analyzed and evaluation of individual structures, like the muscle, the valves, the papillary muscles, etc., can be done. The amplitude mode (or the A-mode) is no longer used and the B-mode, often strategically combined with color, gives a good 2-dimensional view of the underlying cardiac structures. The M-mode or the motion mode is used mainly for the evaluation of contractility, valvular function and leaflet coaptation. The combination of color in the M-mode also gives the perspective of flow direction across structures. Tissue Doppler or spectral ultrasound imaging along with 3-D echocardiography with color rendition are recent developments. These help in tissue differentiation and detecting defects.
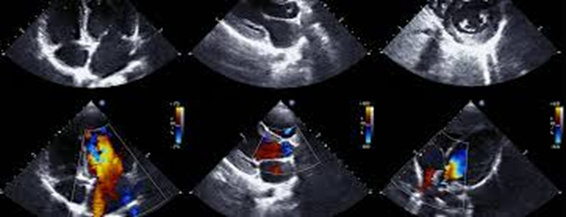
In ischemia the common finding is a regional wall motion abnormality (RWMA). This depends upon the area of circulatory mismatch in demand and supply of that area. Global reduction in muscle contraction raises the suspicion of coronary insufficiency and further investigations are warranted. Stress echocardiography with the inotrope dobutamine helps in identifying regional myocardial viability and myocardial thickening in such a test is heartening. The test should be performed by a qualified person capable of managing emergencies.
Traditionally trans-thoracic echocardiography (TTE) is done in the preoperative decision-making period and if any suspicious event is noticed, like global ischemia or an associated defect, a trans-esophageal echo-cardiogram (TEE) is advised. In coronary artery bypass surgeries (CABG) the use of TEE should be considered to confirm the preoperative diagnosis, detect new pathology, adjust the surgical plan, or to assess surgical intervention. In some cases, the intra-operative hand-held echocardiographic vascular probe may be used to scan the arteriosclerotic plaque conditions of the coronary stenoses and an epiaortic scan of the ascending aorta can also be done for a decision for the aortic involvement of proximal anastomoses.
3. CT-angiogram:-- Computed cardiac CT-angiogram has now become one of the most sought after diagnostic investigations. CT-angiogram is only one part of the tomographic package. As only a small amount of a low-iodine containing dye is used by the peripheral intravenous route, the procedure is better accepted by patients also. Excepting the slight risk of radiation, the procedure is not only safe but also provides a comprehensive information about the cardiac structures, size and sites of aneurysms and dissections, calcium score in atheromatous coronary stenosis, etc.
The physician should be aware that the minimal requirement is a 64-slice helical (or spiral) CT-scanner and the application for 3-D volume rendition. An added advantage is the simplified 3-D rendered photograph of the heart in several positions for visualization of the epicardial length of the coronary arteries.
CT-scan is the chosen method in post-operative cardiac cases due to the presence of stainless steel wires or bands used for sternal apposition and other metallic clips for occluding bleeding vascular branches that may develop magnetic properties over time.
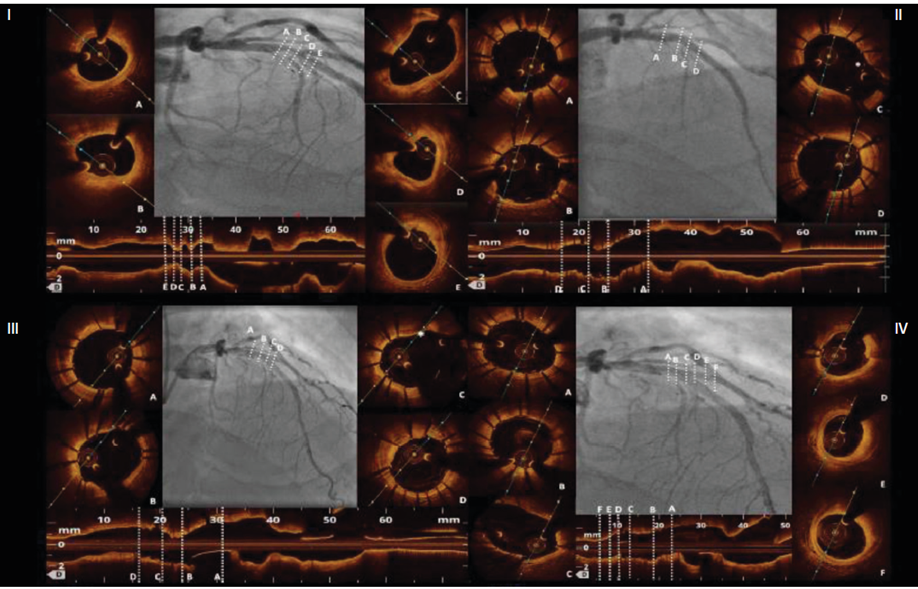
4. Cardiac catheterisation, dynamic angiography :-- There was a boom in cases for revascularization, both by surgery and catheter based balloon angioplasty with stenting. Of late it is appearing such that often some stenosed vessels not requiring a restoration of flow as, though stenosed, the native flow in such vessels often equals or surpasses the bypass graft flow. This is found more often with pedicled arterial conduits, and the effect of this competitive flow leads to a withering of the graft most commonly closed of those venous terminal bypasses where the anastomosis was inadequate. Again circulatory restoration by any means requires a cardiac catheterisation and selective coronary angiography. The iodinated dye used in angiography highlights the epicardial vessels and shows as a luminogram contouring the stenoses on the way. Total blocks are shown as sudden cut-off. Every operator has a strategy for revascularization. This is particularly true for multi-vessel disease and multi-vessel grafting became a norm. Among surgeons LIMA to LAD and venous graft to every other angiographically demonstrated focally narrowed epicardial artery, individual or sequential, was the common practice. At this stage vessel size was not a consideration and the practice of endarterectomy was individualized. Lengthening of the arterial conduit by anastomosing RIMA with a pedicled LIMA, either Y or a T-fashion and sequential side-to-side with end-to-side anastomosis of the conduit and the target coronary artery beyond the stenosis, became the basis for total arterial revascularization. In spite of the reservation for a single pedicle for the total arterial anastomosis, this procedure is becoming commoner in the beating heart with the detection of increasing numbers of multi-disease coronary blockages in patients with diabetes, obesity, and genetic predisposition. New conduits like the free radial, the pedicled gastro-epiploic, and a lengthening of pedicled LIMA with a free vein conduit gradually came into practice. Myocardial viability of a region became an important issue and the quantity of flow in the post-anastomotic segment had also to be taken for operative consideration to limit unnecessary grafts.
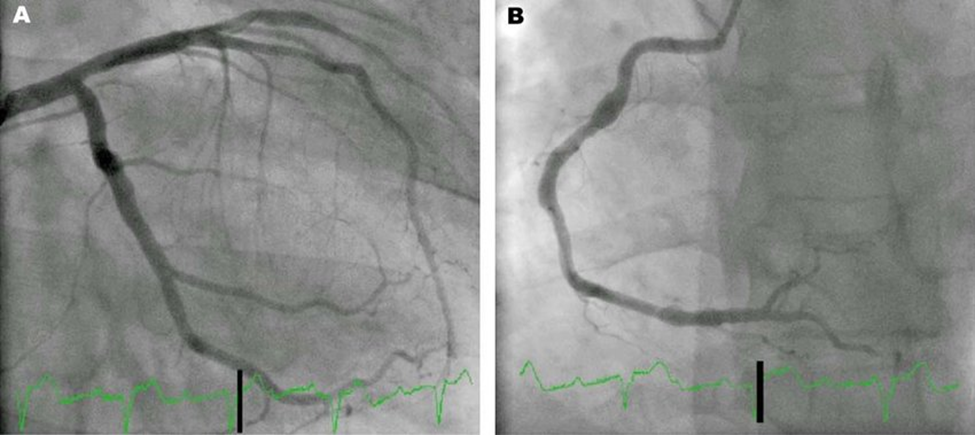
Left coronary arteries Right coronary artery
Nowadays measurement of a catheter based fractional flow reserve is followed by many. FFR provides a reasonable perspective of blood flow to the post-stenotic segment and this is even more advantageous for the PCI physicians as they can take an on-table decision, especially when not to intervene. They also watch for the dye blush and the time taken for washout in the region of myocardium supplied by the catheterised epicardial artery signifying capillary flow signifying a run-off in the coronary microcirculation. This may minimize a no-reflow phenomenon.
Multiple projections at different angles and tilts are normally taken to unmask the overlaps and with the intent to see the full length of the artery.
Periodic guidelines about indications, methods, results, etc. are published from time-to-time. Common people, however, are afraid of the pain, critical nature of the process, other comorbidities, statistical results, and the prolonged time of recovery after surgery even though a physician gives the best option for circulatory restoration, most often PCI is chosen even though trials, blinded and multi-centre, still endorse the durability of surgery. Surgical revascularization has the added advantage of anastomotic revision. Recently the concept of applying the principle of transit time flow (TTF) to assess post-stenotic blood flow in epicardial arteries. So far industry has come up with a hand-held ultrasound probe which works satisfactorily for surface arteries only.
TIMI flow in cardiac catheterization is a risk score favored by interventional cardiologists. A TIMI score represents the perfusion state of the heart that may be associated with re-occlusion, ischemic sequelae, and greater extent of myocardial damage. TIMI Coronary Grade Flow was established to ensure a uniform and consistent method of recording epicardial perfusion on coronary arteriography.
● Grade 0 (no perfusion): There is no antegrade flow beyond the point of occlusion.
● Grade 1 (penetration without perfusion): The contrast material passes beyond the area of obstruction but “hangs up” and fails to opacify the entire coronary bed distal to the obstruction for the duration of the cine-angiographic filming sequence.
● Grade 2 (partial perfusion): The contrast material passes across the obstruction and opacifies the coronary bed distal to the obstruction. The rate of entry of the contrast material into the vessel distal to the obstruction or the rate of clearance from the distal bed is perceptibly slower than its entry into or clearance from comparable areas not perfused by the previously occluded vessel—e.g., the opposite coronary artery or the coronary bed proximal to the obstruction.
● Grade 3 (complete perfusion): Antegrade flow into the bed distal to the obstruction occurs as promptly as antegrade flow into the bed proximal to the obstruction, and clearance of contrast material from the involved bed is as rapid as clearance from an uninvolved bed in the same vessel or the opposite artery.
Frame count is employed to measure the number of cine-angiographic frames to reach standardized distal landmarks. This provides a quantitative assessment of epicardial flow and enhances the reproducibility of the angiographic assessment.
Left ventriculography is done whenever an echo shows RWMA or global hypokinesia and surgical teams practicing arterial revascularization always prefer a LIMA shot to avoid the possibility of a ‘steal’.
In rare situations, the introduction and engagement of selective coronary catheters can be difficult. A consequent aortic root angio might suggest a single origin of the coronaries. This situation is dangerous for interventional cardiologists as sudden death due to a massive infarction is a distinct possibility. Lipton Yamanaka first proposed a classification 0f such single coronary systems. This was subsequently modified and the following image is an example of such systems :--
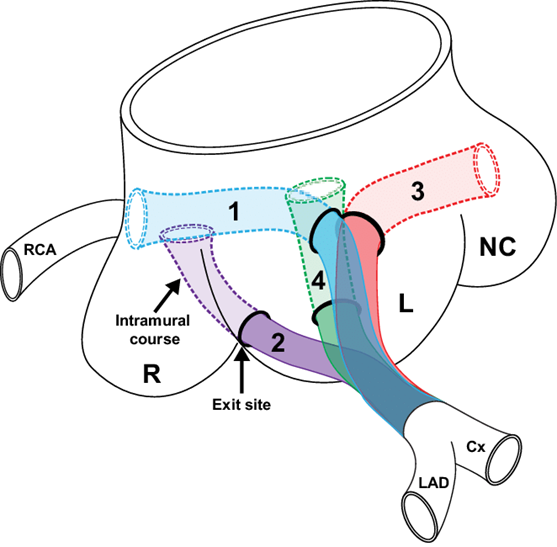
Anomalous origin from the main pulmonary artery is another life threatening condition and angiography is the only quick way for diagnosis and treatment.

5. Intravascular ultrasound (IVUS) : -- A specialized trans-catheter probe with an ultrasound transducer at the tip gives useful images of the interior of the epicardial coronary arteries. Nature and quantification of plaque material is an advantage over conventional catheterisation techniques.
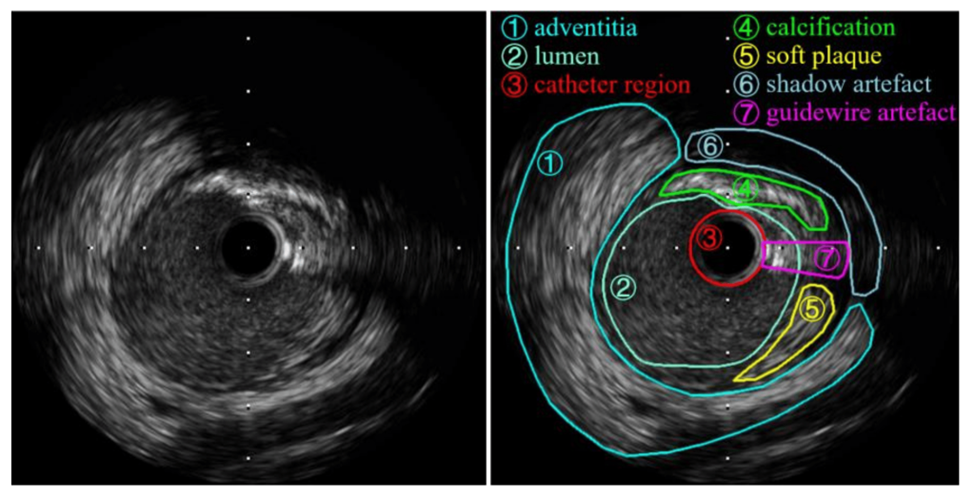
6. Optical coherence tomography (OCT) : -- Optical coherence tomography (OCT) is also a diagnostic procedure used during catheterisation like IVUS. OCT uses near-infrared light to create images of the inside of the coronary arteries. The technique delivers very high-resolution images. The process is 10 times more detailed than IVUS, has a lower depth penetration (1-2 mm compared to 5-6 mm), and can be combined with angioplasty followed by stenting. OCT images help cardiologists see if a stent is opening the lesion and also maintaining the open position for blood to flow. Determination of the nature of atherosclerotic plaques and the endothelial calcium load is an added advantage. OCT also allows precise measurements before and after placing stents.
7. Viability studies :-- Several patients of coronary insufficiency come to the doctor with features of either impending or frank heart failure. Some even have a history of an event of acute coronary syndrome. A massive infarction will lead to death and there has to be enough contractile tissue in the ventricles to overcome the circulatory vascular resistances. Whenever the left ventricular ejection fraction is <40, heart failure is imminent and is written as a heart failure with reduced ejection fraction (HFrEF). Some amount of heart muscle is essential for sustenance of contractility forceful enough to drive the circulation forward and perfuse the vital organs. Echocardiography not only gives an idea of the global ejection fraction, but also an idea of the nature of wall motion abnormalities of the heart after an insult. The reduced ejection fraction in the compromised heart in coronary insufficiency can be as follows :
● Only a region of myocardium affected by the sudden insult. This patch of myocardium is viable but "stunned" or "hibernating". This patch may be poorly contracting, not in synchrony with other areas, akinetic, or dys-synergic.
● Global hypokinesia in multi-vessel disease.
● Global hypokinesia due to septal infarction and paradoxical septal motion.
● Total or partial infarction of the regional muscle mass. Akinetic full thickness infarction of regional cardiac tissue appears thin on 2-D echocardiography.
Viability studies become important here and help planning the circulatory restoration and to find out the extent of myocardial dysfunction. A brief review of the various investigative procedures for myocardial viability is discussed as follows :--
● Dobutamine stress echocardiography : Naturally this procedure comes to the mind first as such patients are managed by cardiologists and the usual ICU appliances are needed. The performing cardiologist is capable of handling emergencies if they happen. Dobutamine is infused at a rate of 2.5 to 10 micrograms/kg/min followed by a high dose (10 to 40 micrograms/kg/min). At low doses this causes an increase in thickness of cardiac muscle implying viability. At the higher dose (10 to 40 micrograms/kg/min), initial viable muscular contraction is followed by diminution of the contractile response -- a typical biphasic response due to a mismatch in demand and supply
● Single photon emission computed tomography (SPECT) with radiotracers : A single photon emission computed tomography (SPECT) scan is an imaging test that detects and measures blood flow in organs. Radioisotopes typically used are iodine-123, technetium-99m, xenon-133, thallium-201, fluorine-18, and the newer monoclonal antibody or nanoparticle labeled agents like 89Zr-DFO-trastuzumab. Other examples of commonly used radioactive tracers include rubidium-82, 13-N ammonia tritium, carbon-11, carbon-14, oxygen-15, fluorine-18, phosphorus-32, sulfur-35, iodine-123, and gallium-67. Of these, technetium-99m is used mostly because of the short half life and ease of disposal. Xenon is a gas and suited for lung perfusion studies most but the image resolution is not satisfactory. So far experimental mouse-model research with 89Zr-DFO-trastuzumab in intra-operative HER2/neu positive breast tumors with an emphasis on the bio-luminant extent of the growth is of interest only. SPECT with technetium-99m is for preoperative assessment, while that with the monoclonal antibody tracer emphasizes real-time intraoperative resection of malignant masses.
A). Technetium 99m Sestamibi SPECT scan is done commonly for cardiac viability. Tc-99m Sestamibi, a cation, having the ability to diffuse across cell membranes into the mitochondria. Positive uptake is suggestive of viable myocardial cells. Normal uptake is consistent with viable myocardium, moderate uptake is consistent with a mixture of infarct and viable tissue, and absent uptake is consistent with an infarct.
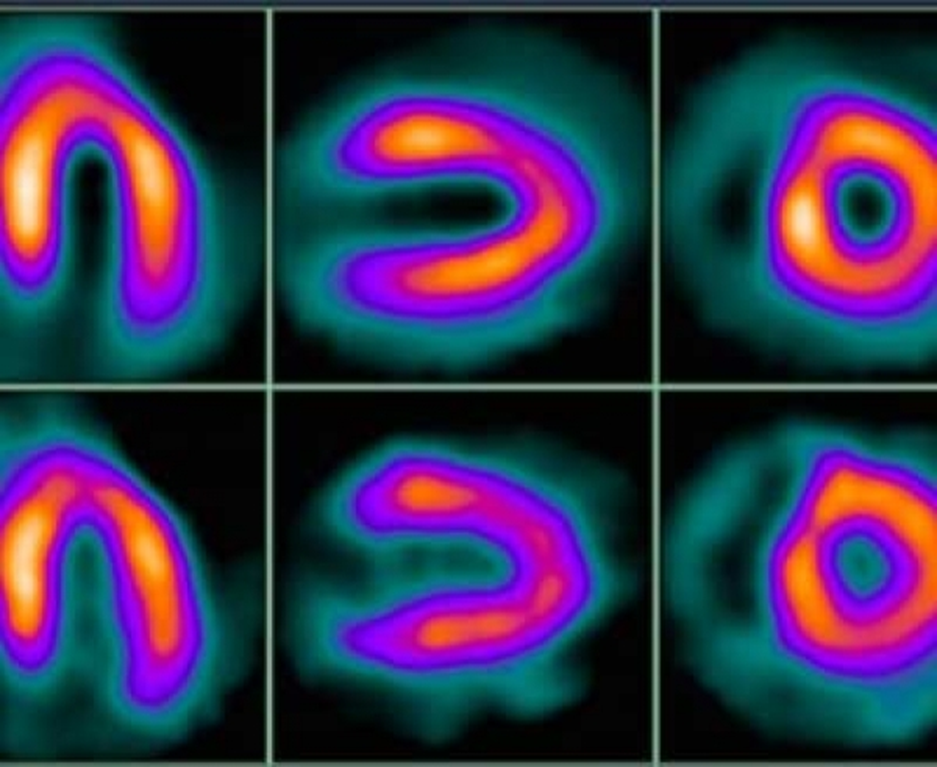

Schematic guide for understanding SPECT.
B). Thallium-201 Single Photon Emission Computed Tomography (SPECT) scan actually acts by replacing k+ and the integrity of the cell membrane in living myocytes indicates viability. 85% of this radiotracer is taken up by life myocardial cells during the first pass and a concentration difference of the tracer in myocardial cells and blood not washed out in the first pass is measured. Here more Th 201 activity suggest a low washout thus indicating ischemia. Reinjection of the tracer and the subsequent redistribution may actually increase the specificity of this test to some extent.
C). 18-Fluoro-deoxyglucose is a metabolic radiotracer. Cardiac scanning with this material is complex, combining detection of the radiotracer (PET) and CT scan. The metabolic radiotracer 18 FDG is injected. Normal contracting myocardium will show FDG uptake with glucose infusion only and the comparable flow uptake with the tracer used will be normal. A hibernating myocardium will show an absence of uptake for both, while in the ischemic myocardium, the flow uptake will definitely be reduced while FDG uptake is patchy, indicating some degree of aerobic metabolism. In summary, this process and the interpretation of results is complicated and recommended for early detection of sarcoidosis, atrial tumors, and other malignant lesions of the heart.
8. Cardiac MRI : – The myocardial viability involves a set of different MRI sequences for the assessment. Every aspect of 3-Tesla MRI in T1, T2 planar images with specific angles for MRI (e.g., axial angular and diaphragmatic, ,horizontal long axis or 4-chamber, vertical left ventricular long axis or 2-chamber, sagittal left ventricular outflow tract (LVOT) or 3-chamber, and short-axis view (sax)), mapping and stress perfusion, cine MRI imaging, perfusion imaging and early and late gadolinium enhancement). Contrast enhancement further helps in tissue differentiation. A gated ECG should always be the target. Though suggested results are satisfactory, the prolonged time and the test conditions mandate that such an investigation should be performed only on patients with a stabilized heart failure who does not have claustrophobia.




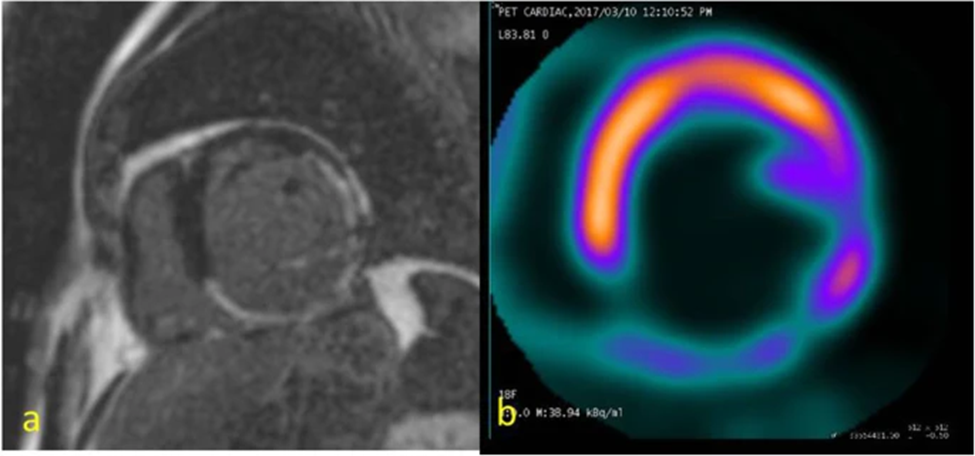
A patient with triple vessel disease.
a) Free-breathing delayed by contrast-enhanced MRI in short-axis view reveals late gadolinium enhancement in < 50% myocardial thickness suggestive of subendocardial infarct in left circumflex and late gadolinium enhancement in complete thickness of right coronary artery territory suggestive of transmural infarct.
b) FDG PET reveals normal uptake in left anterior descending artery < 50 %uptake in the right coronary artery territory and > 50 % uptake in the left circumflex territory. Practically, those involved with revascularization, both surgical CABG and PCI, do not show such concern and have the hope of recruitment of as much stunned and hibernating myocardium as is possible in order to enhance the ejectile performance of the heart. Viability investigations are seldom advised and mist of the decisions are made on the basis of an ECG, an echocardiography, and a conventional dynamic angiogram preceded by cardiac catheterization. When a patient comes to the specialist with the specific complaint of precordial pain appearing with effort, altered lipid profile raising the suspicion, an altered ECG without or with minimal non specific symptoms, episodes of pedal edema and heart failure that can be easily controlled but not explained, etc., directed investigations following a logical sequence should be advised in the following manner:
ECG ⇒Altered or normal⇒TMT or stress ECG⇒Echocardiography for wall motion abnormalities and ejectile performance of the heart⇒ cardiac catheterization and angiography ⇒revascularization.
Before the introduction of cine recordings, the term ‘gated’ was borrowed from the industrial parlor, and thus a gated CT, or a gated MRI, or a multi-acquisition gated (MUGA) scan came to be known in the medical field. To simplify gated scans are generally indicated for organs that are functionally affected by movement and a gated scan is able to report the peak functioning ability and the dimensions of the organ. ECG gating is commonly done in gated CT or MRI scans giving an idea of the rate and contractile phase.
Tagged tracer or radionuclide blood pool scan and multiple exposure acquisitions at different phases of movement, e.g. systole and diastole of the heart, respiratory movements, and nature with blood flow, characterize a MUGA scan. Present studies show that even if a MUGA scan gives a better idea of contractile and dimensions of the heart, this is done rarely. Heart is the only organ evaluated nowadays, especially in cancer patients, for early detection of chemotherapy induced diminution of cardiac contractility. Cost is another factor.
A brief understanding of the venous drainage of the heart is necessary for physicians involved in restoration of coronary flow. The main differentiating point is the fact that though the majority of the venous channels accompany the principal coronary arteries as accompanying veins, at times as two parallel veins along the arteries, there are two systems of venous drainage. The two distinct systems are in short : –
1). greater cardiac venous system, and
2). the smaller cardiac venous system.
The greater cardiac venous system returns three-quarters of the deoxygenated blood from the myocardium to the cardiac chambers and this includes the coronary sinus and its tributaries, marginal veins, anterior cardiac veins, middle cardiac veins, ventricular veins, and atrial veins. The 2nd system, or the smaller cardiac venous system, is responsible for the return of one-quarter of the deoxygenated blood from the inner layers of the myocardium to the cardiac chambers. This system is mainly composed of Thebesian veins draining deoxygenated blood from all sections of the myocardium chambers. Thebesian veins also drain the right side of the heart more than the left side.
As of now the following is a concept only and patient selection with identification of beneficiaries have not been sorted out yet.

The arteries and veins create a rich system of intramyocardial network of arterioles capillaries and venules visible as blushes at selective angiography. These are responsible for the near-total O2 extraction by the cardiomyocytes. There is a proposal for the transcatheter creation of an arteriovenous communication with the hope that the higher arterial blood flow will reverse and flood the capillary system. This proposition is for cases where surgery under anaesthesia is risky and other comorbidities make the patient unfit.
This is a compilation of the essential basics for a cardiac surgeon to know before starting coronary revascularization.



Comments